- What is ePrescribing?
- Benefits
- How does ePrescribing work?
- Don't forget
- Set up requirements
- Training and support
What is ePrescribing?
Electronic prescribing is when the entire prescription and dispensing process is electronic, no paper needed.
Although the basic technology and infrastructure for the process has existed for a few years, there was still a legal requirement (under the Pharmaceutical Benefits Scheme) for a hardcopy script to be printed, before the medicine could be supplied. This legislation was updated by the Australian Commonwealth government on 31 October 2019, paving the way for implementation of ePrescribing nationally.
For more information, see the Australian Digital Health Agency's ePrescribing information for prescribers and dispensers respectively.
Benefits
- Improved patient safety – reduced risk of transcription errors.
- Workflow benefits – prescribers will no longer need to print and sign prescriptions.
- Increased convenience and flexibility for patients.
- Supports telehealth consultations and potentially other digital health initiatives.
- Reduced medication misuse through increased data available for real-time monitoring of prescriptions.
How does ePrescribing work?
An electronic prescription is created from within the prescriber's clinical software. The e-script is then sent to the Prescription Delivery Service, similar to the process for Electronic Transfer of Prescriptions (ETP).
There are two main options for an electronic prescription.
Option 1 (Token model)
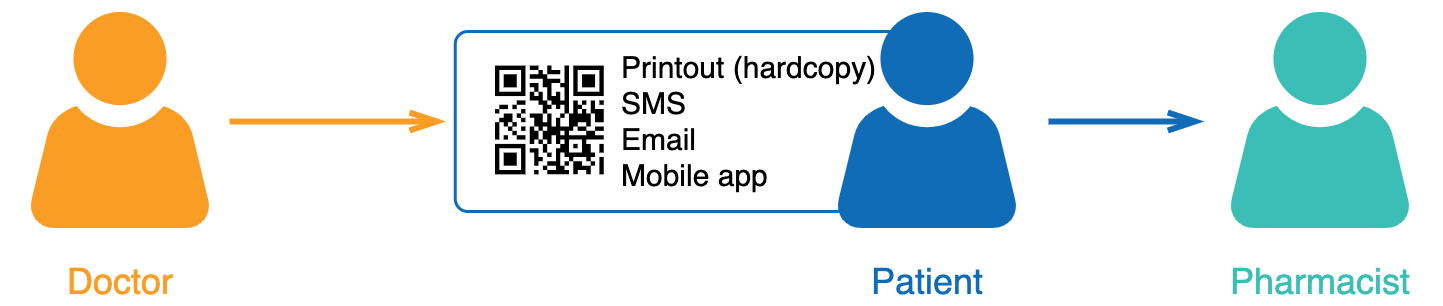
- The script can only handle one medicine.
- If the patient is prescribed more than one medicine, then a script for each medicine will need to be created.
- Patient receives a QR code (i.e. the 'token') via SMS, email, or mobile app. Alternatively, the prescriber can print out the QR code and hand to the patient.
- Patient then sends or brings in the QR code to the pharmacy.
- Pharmacist scans the QR code to retrieve the script.
- If it is a repeat script, the pharmacist will be able to issue a new token for the next script.
- This model was fast-tracked to support the use of telehealth consultations. Most general practices and community pharmacies now have this function made available to them.
Option 2 (Active Script List model)

- Can handle more than one medicine.
- Does not require the patient to send/bring a QR code.
- Patient registers for Active Script List (ASL) at their preferred pharmacy.
- Electronic scripts are issued and added to a list of 'active' prescriptions (unless patient requests otherwise) and these are then available for dispensing. Note: Prescriptions issued on paper with a barcode (ETP) will also appear in the ASL.
- Before dispensing, the pharmacist must register the patient to their active script list and the patient must provide consent (most likely via SMS or email).
- Patient attends the pharmacy, the pharmacist identifies the patient, and then accesses their active scripts.
- This model is now available and patients requiring multiple medications are encouraged to talk to their pharmacist about using ASL.
Printed prescriptions
Paper prescriptions will continue to be an option. Use of paper or electronic will depend on the capability of the prescribing software and the patient's preference.
It will not be possible to create both an electronic and paper version of the same script (i.e. one method must be chosen at a time).
Don't forget
- Keep up to date SMS/email contact details for patients.
- Electronic prescriptions are an alternative to paper.
- Prescribers should consult with their patient about whether an eScript is the best option, particularly if they're using the Token (see above) and the patient has multiple medications.
- If a patient’s preferred local pharmacy is not ready for electronic prescriptions, prescribers can elect to print out a paper script.
- In most circumstances, digital 'tokens' should be sent to the patient/carer/agent and not directly to their pharmacy.
- However, in some situations (e.g. RACFs/owing scripts/S8 dosing points) a paper prescription would normally be sent directly to the pharmacy. And this is also acceptable with digital 'tokens' on the proviso that it reflects the choice or best interest of the patient/agent/carer and as such facilitates the most timely and convenient access to the prescribed medicine.
- It is important that such arrangement are organised in consultation with the pharmacy.
Set up requirements
There are 3 main requirements for ePrescribing to work.
1) Healthcare Identifiers Service
You must be able to connect to the Healthcare Identifiers Service. If you can access records in My Health Record, then you're already set up. If not, see set up steps for the HI Service below.
2) Electronic Transfer of Prescriptions
Have a Prescription Exchange Service installed (see Electronic Transfer of Prescriptions).
3) Latest version of your software
The latest version of clinical software with electronic prescription capability. Your vendor should be in touch with you about when their system is likely to be ready.
Set up steps for Healthcare Identifiers Service
The HI Service requires:
- your clinic or pharmacy to have been issued with identifiers for your organisation and for your prescribing or dispensing clinicians.
- a current NASH certificate
Training and support
- Visit the Australian Digital Health Agency's training portal for free CPD-accredited online training modules explaining electronic prescriptions and the Active Script List.
- View on-demand webinars to learn more about using electronic prescriptions.
- Contact your local Primary Health Network for further support.